Will Patients Shape the Field of Precision Medicine?
How Patients COULD Shape Precision Medicine
I believe that we're at an incredibly important inflection point in the exploding field of Precision Medicine. Proactive patient participation could shape this nascent industry. If the patients who benefit the most from Precision Medicine also become empowered and engaged patients, rather than scientific guinea pigs, we are more likely to make very rapid progress in identifying gene mutations that cause disease and in preventing or reversing the damage they do.
In January 2016, both the US government and the Chinese government amplified their rhetoric about investing in Precision Medicine.
In the US, during his State of the Union speech in 2016, President Obama pronounced the the USA would be the country to "end cancer," annointing VP Joe Biden to lead the charge and citing Precision Medicine as one of the key enabling technologies. This cancer-specific challenge built on Obama's call to action in his 2015 State of the Union address, in which Obama proclaimed: “Tonight, I'm launching a new Precision Medicine Initiative to bring us closer to curing diseases like cancer and diabetes — and to give all of us access to the personalized information we need to keep ourselves and our families healthier.” Obama pledged $215 million
In China, the details of the government initiative will be released in March, 2016, after the government approves its next five-year plan. But the word is out: "Officials have declared precision medicine – a customized form of health care based on genome-sequencing technology – as one of the nation's foremost science and technology projects under the 13th Five-Year Plan for the 2016-20 period." Chinese universities and research institutions are already announcing their programs for 2016, anticipating government research funding on the order of 60-billion yuan (US$9.2-billion) budget spread over the next 15 years.
According to an article in Nature, China Embraces Precision Medicine on a Massive Scale, "this figure is not finalized, cautions Zhan Qimin, director of the State Key Laboratory of Molecular Oncology at Peking Union Medical College in Beijing ....who is involved in the initiative...He says that the effort will consist of hundreds of separate projects to sequence genomes and gather clinical data, with support for each ranging from tens of millions of yuan to more than 100 million yuan." The Nature article explains:
"Anticipating the initiative, leading institutes — including Tsinghua University, Fudan University and the Chinese Academy of Medical Sciences — are scrambling to set up precision-medicine centres. Sichuan University’s West China Hospital, for instance, plans to sequence 1 million human genomes itself — the same goal as the entire US initiative. The hospital will focus on ten diseases, starting with lung cancer.
Both the US and the Chinese efforts will focus on genetic links to diseases that are particularly deadly, such as cancer and heart disease. But China will target specific cancers, such as stomach and liver cancer, which are common there."
Chinese Experts on using Precision Medicine to Treat Non Small Cell Lung Cancer at a conference in the Fall of 2015. (A) Prof. Haifeng Wang, Shanghai Pulmonary Hospital, Tongji University; (B) Prof. Hao Long, Director of Lung cancer institute, Sun Yat-Sen University; (C) Prof. Ying Chai, Director of Thoracic Surgery, Second Affiliated Hospital of Zhejiang University; (D) Discussion Guests(from left to right): Kaican Cai, Jianyang Liu, Xiaofeng Chen, Honghe Luo, Chun Chen.

From left, Jieming Qu, Euan Ashley, Guoyuan Yang and Taha Kass-Hout participate in a panel discussion on precision health Oct. 15 at the Sino-U.S. Symposium on Medicine in the 21st Century. The event was held on the Stanford campus at the Li Ka Shing Center for Learning and Knowledge.
Norbert von der Groeben
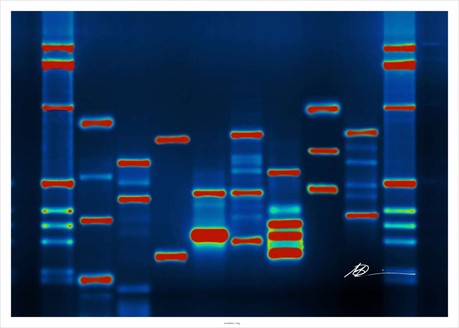
Photo Courtesy of Micah Baldwin via Flickr, CC BY-SA 2.0
The race is on! However, unlike the space race between Russia and the US, dating back to the 1950s, the race to advance Precision Medicine, should, by its very nature, be a collaborative one, in which the figurative baton passes back and forth between scientists around the world as they collaborate to build genomic databases, to aggregate patients' electronic medical records, and to identify, at the molecular level, treatments that work and treatments that don't.
What is Precision Medicine?
The term Precision Medicine is becoming more popular than the term "personalized medicine" because it does not necessarily imply that each therapy or treatment is targeted for a specific individual, but rather for a cohort of people who share specific genes, as well as clinical histories, and environmental factors. Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease, produced by the National Research Council in 2011, the glossary entry for Precision Medicine "refers to the tailoring of medical treatment to the individual characteristics of each patient. It does not literally mean the creation of drugs or medical devices that are unique to a patient, but rather the ability to classify individuals into subpopulations that differ in their susceptibility to a particular disease, in the biology and/or prognosis of those diseases they may develop, or in their response to a specific treatment."
But, I also like this definition from Mikael Dolsten and Morten Sogaard, from their seminal paper published in May 2012, which elucidates the relationship of Precision Medicine to Personalized Medicine:
Precision Medicine is an approach to discovering and developing medicines and vaccines that deliver superior outcomes for patients, by integrating clinical and molecular information to understand the biological basis of disease. This approach leads to better selection of disease targets and identification of patient populations that experience better clinical outcomes. Ultimately, the potential of Precision Medicine is that it will yield treatments that deliver clinically significant treatment effects, with favorable safety profiles. When appropriate, these new treatments are focused on a particular sub-group of patients with certain genotypic and/or phenotypic characteristics that make them more likely to benefit or less likely to experience side effects. A related concept, 'Personalized Medicine', has been defined by President’s Council of Advisors on Science and Technology (PCAST) as 'the tailoring of medical treatment to the individual characteristics of each patient to classify individuals into subpopulations that differ in their susceptibility to a particular disease or their response to a specific treatment. Thus, products and diagnostics developed through Precision Medicine facilitate the practice of Personalized Medicine."
Technologies Shaping Precision Medicine
I am admittedly ill-equipped to chronicle all the technologies involved in the evolution of Precision Medicines. But, here's my first pass at identifying some of the technology enablers that are accelerating interest by corporations, governments, research institutions, healthcare providers, healthcare payers, caregivers, and patients (in approximately that order of skin in the game). They include:
- Genomic sequencing
- Cell signaling technology
- Discovery and development of biomarkers and diagnostic markers
- Big Data analysis
- Electronic Medical/Patient Records
- Mobile Health Monitoring applications
Ethical Issues Shaping Precision Medicine
How Patients COULD Shape Precision Medicine
I believe that we're at an incredibly important inflection point in the exploding field of Precision Medicine. Proactive patient participation could shape this nascent industry. If the patients who benefit the most from Precision Medicine also become empowered and engaged patients, rather than scientific guinea pigs, we are more likely to make very rapid progress in identifying gene mutations that cause disease and in preventing or reversing the damage they do.
Why Kids' Cancers Have Higher Success Rates

Photo: Courtesy of St. Jude's Chidren's Research Hospital
Allie Johnson, a cancer patient at St. Jude's Childrens' Research Hospital
What we've learned from the treatment of cancer in children is that collaborative cross-disciplinary research and treatment are essential to delivering successful outcomes. Most pediatric cancer patients participate in clinical trials and provide consent for researchers and clinicians around the world to observe and comment on their treatment regimes. This global, cross-disciplinary sharing and learning have accelerated progress.
In an article in Popular Science, titled We are Astonishingly Good at Treating Childhood Cancer, Why?, Alexandra Ossola writes: [The emphasis is my own]
"Childhood cancers are rare diseases, affecting around 16,000 children and adolescents per year but making up only 2 percent of all cancer cases. Over the past three decades, this collaboration has coalesced most clearly in clinical trials. About 60 percent of all kids with cancer participate in clinical trials, and have done so for decades. 'Every child we treat is an opportunity for us to learn and in that way continually optimize our treatments,' says Andrew Kung, the head of the Pediatric Hematology, Oncology, and Stem Cell Transplantation Division at New York Presbyterian Hospital, ...Unlike for adult patients, fewer than 5 percent of whom are enrolled in clinical trials, these are the norm for children."
“'We can’t get anything done as pediatric oncologists unless we work together, pool our results and talk to each other,' says Crystal Mackall, the chief of pediatric oncology at the National Cancer Institute. 'Over and over again, the principles that childhood cancer teaches us turn out to be fundamental. This ability to use cooperative groups to learn about rare diseases is an important insight, as adult doctors are coming to understand.'"
"'Because of kids’ fast metabolisms and general lack of other health issues, kids can tolerate a much higher dose of treatment,' explains Andrew Kung. 'If you come to our clinic, you see the kids running around, and you would not know that these are kids with cancer, except that they are bald. Whereas adults getting the same kinds of therapies would be laid up in bed.'”
"Over time, researchers have found that this biology makes kids’ cancers much more treatable, contributing to the 80 percent cure rate. But to be able to leverage these elements of biology, researchers first had to discover viable treatments."
As a result of the systematic testing and constant collaboration, many of the treatments found to work in kids have been extrapolated to adults. In a sense, all cancer patients have benefitted from pediatric oncologists’ decades of work.
Upcoming Events

A free virtual seminar on Precision Medicine will be held by LabRoots on Wednesday, February 24, 2016. You can see the agenda and register for the event here. The event is sponsored by Chemical & Engineering News. (Please note all times are PST).
0 comments
Be the first one to comment.